Treatment of the knee joint
The International Center for Orthopedics at the ATOS Clinic Heidelberg specializes in the treatment of the knee joint. The knee is the largest and most complicated joint in the human body. It is stabilized by ligaments and the joint capsule and has little bony support. Therefore, it is particularly sensitive, prone to injury and painful.
Learn below how to recognize a foot injury or disease and have it treated properly. What symptoms should you look out for and when is the best time to see a specialist? You can also find out what treatment options are available today and what rehabilitation can look like afterwards.
Knee injuries and diseases
Gonarthrosis (wear and tear of the knee joint)
What is gonarthrosis?
In knee joints, a severe abrasion of the cartilage to the bone is called gonarthrosis. It is now the most common disease of the knee joint.
Increased body weight might play a role in the formation of arthrosis. But also congenital or acquired malpositions of the legs, as well as instabilities or injuries lead to wear and tear of the cartilage. Meniscus damage, torn ligaments, unilateral loads and other factors increase the risk of developing gonarthrosis.
How to notice osteoarthritis of the knee? What are the typical symptoms?
With gonarthrosis there are various complaints: slightly noticeable pain in the knee during movement and sometimes when resting. The mobility of the knee is significantly limited. Swelling, muscle tension or even audible joint grinding occur. In all cases, an experienced physician should be consulted.
How can gonarthrosis be diagnosed?
Clinical examination and state-of-the-art imaging such as ultrasound, X-ray, DVT, CT and MRI reveal information about the extent of cartilage damage and the severity of arthrosis.
Can arthrosis of the knee be treated without surgery?
Conservative therapy involves physiotherapeutic measures and the use of medication. Injections or autologous blood (ACP) therapies reduce pain in the knee, but cannot significantly stop the progression of the disease. The most effective conservative measures are weight reduction and sports. High-impact sports, such as soccer and squash, should be avoided; in their place, it is better to practice low-impact sports, such as cycling, rowing, swimming, walking, cross-training, and stepping. It is important to exercise in the low level of pain.
Which therapy methods are recommended?
Because gonarthrosis is a wear and tear of the joint that has often left visible damage, it may be recommended to clean out the knee joint using knee arthroscopy – especially if mechanical blockages (e.g., free joint bodies, interfering bone edges, pinching meniscus or cartilage) are found. If the gonarthrosis is already severely advanced, this method will not be very helpful. In that case, the worn joint surface can be partially (sled prosthesis) or completely (total knee arthroplasty) crowned. Depending on the severity of the gonarthrosis, the experienced specialist must determine which therapy is optimal. In both cases, the patient can recover quite quickly and return to active daily life.
Why it is important to do muscle training after the surgery?
Mobilization is started directly after the operation. During rehabilitation, the patient executes a special program focused on the new joint.The surrounding musculature is strengthened to avoid malpositions.
Do you have any further questions?
Would you like to learn more or are you directly affected? Then feel free to contact our experts. They will be glad to help you.
Retropatellar arhtrosis
How does arthrosis develop behind the kneecap and what are the possible causes?
Arthrosis can also occur directly behind the kneecap (patella), for example as a result of pressure or high load. This is known as retropatellar arthrosis. The causes are degenerative processes, instability due to low ligament tension, malformations of the patella or the trochlea.
Patella fractures, i.e. fractures of the kneecap, or osteochondral lesions, thats means injuries to the articular cartilage and the underlying bone, can also be the reason.
How do you notice patellofemoral arthrosis?
Anterior knee pain is noticed, especially when climbing stairs, standing up, kneeling or squatting. Occasionally, there is a crunching sound with movement. Often the knee is simply stiff. In advanced arthrosis, the knee may lock, be heated, swollen, and there is knee joint bruising.
What do the clinical examinations look like?
Radiographs (x-ray images), a DVT and a CT scan can provide information about the femoropatellar joint. The joint space can be determined more precisely with the aid of the so-called defilee image (the patient lies with bent legs on the X-ray table). If the gap becomes more and more narrow, it is an indication of cartilage erosion due to malalignment. Magnetic resonance imaging (MRI) also shows damage to the cartilage and can provide additional information.
How can retropatellar osteoarthritis be treated effectively?
In the late 1970s, the replacement of the femoropatellar bearing (patellar back surface and corresponding femoral joint surface) was started with good results. Meanwhile, improved prostheses are available, which take the individual anatomy of the patient into account.
The anatomical guiding of the patella in the bearing is important, in addition to the replacement of the femoropatellar bearing, to provide a central running of the prosthesis in the femoral gliding path without tension.
Do you have any further questions?
Would you like to learn more or are directly affected? Then feel free to contact our experts Professor Siebold and Professor Becher. They will be glad to help you.
Cartilage damage
Why is cartilage damage to be taken seriously?
Untreated joint cartilage defects are problematic because the regeneration of a cartilage proves to be difficult. Today, it is known that injured or destroyed cartilage does not regenerate or grow back to its original shape. Instead, it results in poor quality scar tissue if the cartilage is not treated. Since fibrocartilage is very soft, it tends to wear out rapidly and this can cause arthrosis.
How do you notice cartilage damage in everyday life?
Typical symptoms of cartilage damage in the knee include pain and limited mobility. Depending on the degree of the defect, swelling of the knee may also occur or it may hurt at rest. Crunching and cracking sounds can be heard from time to time. The knee can also lock completely and should then be examined by a specialist at the latest.
What causes cartilage damage?
Causes of traumatic cartilage damage are injuries or accidents, e.g. during physical sports (soccer, handball or ice hockey), but also leisure sports (skiing and snowboarding). Enormous forces are often exerted on the joint, which can lead to cartilage injuries. Severe traumatic cartilage damage occurs frequently, even in the case of fresh anterior cruciate ligament rupture or patellar dislocation. In this case, a piece of healthy cartilage (possibly with bone) can break out of the joint surface, which is known as a chondral or osteochondral flake. Degenerative cartilage damage, on the other hand, can occur as a result of natural wear and tear (genetic influence, stress over decades), with more extensive abrasion of the cartilage covering.
During the clinical examination, how do you recognize a cartilage defect?
With the help of imaging techniques (MRI), cartilage damage can be diagnosed and the appropriate therapy found.
Is it necessary to operate at this point?
No, cartilage damage can often be treated conservatively for years. Therapeutic treatment includes, for example, targeted physiotherapy, cartilage preparations (hyaluronic acid), the body’s own repair enzymes (ACP), medication with an anti-inflammatory effect, and lifestyle adjustments (sports activities, weight).
But when is surgery indicated?
If deep, so-called „cartilage holes “ are present in young patients, surgical treatment is recommended, to prevent a rapid progression to the final stage of arthrosis.
So what to do with freshly sheared cartilage-bone fragments?
After severe knee injuries, a fragment of bone and cartilage may be torn off from the joint surface. X-rays, DVT, CT and MRI can detect this in most cases. With timely surgery, avulsed bone-cartilage fragments can be replaced and fixed in place. Successful restoration of the joint surface is the optimal therapy.
Fig.2: Fresh cartilage-bone defect (left), preparation of the detached fragment (center) and re-implantation and refixation with two resorbable pins (right).
What´s about arthroscopic cartilage cell implantation (ACI)?
Annually, we have more than one hundred minimally invasive cartilage cell transplantations on the knee, making us one of the most experienced cartilage specialists in the world. As early as 2006, we were one of the first centers in Germany to adopt a new approach to autologous cartilage cell transplantation. The procedure, developed by the company co.don® AG (Berlin), makes it possible to implant the cartilage cells in a minimally invasive manner, i.e. arthroscopically. For this purpose, a piece of cartilage only a few millimeters in size is first removed from an area of the knee joint that is subject to little stress in order to cultivate the cells.
How exactly does it works?
In the laboratory, the cartilage cells are combined into three-dimensional spheres (spheroids), with each individual spheroid containing about 200,000 cartilage cells and having a size of only 0.5-0.7 mm in diameter, depending on the degree of maturity. The 3D spheroids are produced exclusively with the patient’s own blood, thus avoiding foreign proteins and side effects.
As soon as the spheroids are in contact with the prepared cartilage defect site during implantation, they are able to stick to the subchondral bone in a mechanically stable manner due to adhesive proteins. In many cases, we treat several defects at the same time by means of cartilage cell transplantation.
How is the cell inserted?
Surgical techniques have now been improved so that the operation can be performed with minimally invasive techniques. The cells are transplanted into all areas of the knee joint, e.g. the femoral condyle, the tibial plateau and also the area of the kneecap.
Scientific research: what does it say? What results can be recorded?
Over the past decades, more than 800 patients with spheroids have been successfully treated with arthroscopic surgery. All patients are followed up after surgery – the clinical results are very satisfying in most cases. In several patients we were able to perform arthroscopic follow-up examinations of the transplanted cartilage after six weeks, four months, nine and 18 months.
Complete defect coverage by the cartilage graft was found in 91% (see published studies). MRI images underline the good clinical results.
What is microfracture and what are its benefits?
During arthroscopy, small holes are drilled into the bone in the area of the cartilage defect using a pointed awl. So stem cells are released from the bone marrow (spongiosa) behind. There is hemorrhage from the bone into the defect area. The blood stem cells stick to the site of microfracture. With relief of the knee joint, these stem cells develop into fibrocartilage after a few months and fill the circumscribed cartilage defect. In many cases, the patient is largely free of pain and able to bear weight for some time.
An advantage of the procedure is that it can be used immediately during arthroscopy. The disadvantage is that only fibrocartilage of poor quality is obtained.
Fig.3: Arthroscopic microfracture with awl (left); opening of the subchondral bone at 4 degrees of cartilage damage (center); and leakage of stem cells from the bone marrow (right).
And what is the alternative to microfracturing?
In this procedure, the exposed bone is refreshed with a milling cutter (arthroscopy). This results in the flushing out of stem cells into the defect area and a regenerate of fibrocartilage can develop.
What is the AMIC procedure?
The AMIC procedure is a further development of microfracturing. What exactly is meant by it and what advantages it has for the patient are explained in this section.
What is mosaicplasty?
In mosaicplasty, the cartilage defect together with an underlying cylinder is punched out in a round shape and replaced by a second autologous round cylinder with an intact cartilage surface. The procedure is demanding and very sensitive and requires precise surgery with exact reconstruction of the joint cartilage level.
Do you have any further questions?
Would you like to learn more or are you directly affected? Then contact Prof. Siebold and Prof. Becher directly. They will be glad to help you.
Meniscus injuries
Where exactly is the meniscus located and what is its function?
The meniscus tissue is elastic and lies like a disc between the femoral condyle and the tibial plateau. There is an inner and outer meniscus. The cartilaginous meniscus tissue is the most important buffer during impact loads on the knee.
The meniscus has many functions. By increasing the surface area, the total load is divided on the knee joint. It is responsible for the arsorbtion, for the synovial fluid and stability of the knee joint. This makes the menisci in the knee joint the most important protection for the articular cartilage.
Whats the material specificity of the meniscus?
The meniscus has a dense fibrous tissue that is supplied with blood only at the edge to the joint capsule. This zone is called the red-red zone. There are no nerve fibers and therefore no pain is initially felt with degeneration or injury. However, a degenerative or acute rupture of the meniscus causes displacement and entrapment of meniscal tissue. Weight bearing changes and irritation of the synovial membrane occurs.
Why does a meniscus tear and can it heal again?
Fresh meniscal tears in young patients usually have a good chance of healing. Of course, healing depends on the shape of the tear. Every tissue is subject to natural aging, including the meniscus tissue. Genetic factors play an important role here. The natural aging process is obviously affected by the degree of stress in everyday life.
What are the differences?
Generally poor blood supply to the meniscus means that only healthy meniscal tissue has a sufficient chance of healing in young patients. Tears close to the capsule as well as a meniscus tear in combination with an ACL injury have particularly good healing prospects. In the case of degenerative changes, however, it becomes difficult because there is no healing and thus no reduction in pain.
Which are the consequences of a meniscus tear for the knee joint?
An acute or degenerative meniscus injury should in any case be clarified by a knee specialist in order to initiate an early individual therapy.
Ruptured meniscus leads to a disturbed sliding surface between the upper and lower leg. It can also entrap loosened parts of the meniscus, causing high stresses between the cartilage of the upper and lower leg and destroying the sensitive cartilage surface.
What happens to the cartilage surface if a ruptured meniscus is not repaired?
The once very smooth surface of the cartilage becomes dull and softened. That‘ s the starting point for a gradual defibration and abrasion of the cartilage. We speak of arthrosis when the cartilage has worn down to the surface of the bone. The wear and tear can go unnoticed for a long time until it finally triggers pain.
Why do especially athletes have problems with the meniscus? In what way does a tear occur?
Sportsmen and women often suffer an acute meniscus tear as a result of excessive stress on the meniscus. Patients usually describe a stabbing pain in the knee. Fresh injuries often lead to an acute functional limitation in sports or to a permanent inability. Due to the complaints, the diagnosis of the meniscus lesion is made at an early stage and surgical therapy is initiated immediately. If the fresh meniscus injury is not treated, mechanical irritation and pinching of the meniscus can cause damage, as well as damage to the articular cartilage with early arthrosis.
What are the symptoms of a meniscus tear?
With degenerative tears of the meniscus, the process develops gradually, so that disorders are only noticed after a while. An accident does not always have to be the cause.Everyday stress, e.g. getting out of the car or going into a deep squat, is enough to suddenly trigger pain from the already degenerative meniscus.
On what do you have to pay attention?
If a flap tear or a basket handle tear occurs, acute painful locking of the knee joint with restriction of the range of motion may occur. In most cases, there is a painful inhibition of extension, which can be temporarily relieved by certain rotational movements with reduction of the meniscus. A snapping of the meniscal flap is also described by the patient. Everyday loads can be performed on meniscal tears, but patients in jobs where they have to stand a lot complain of pain in the area of the inner or outer joint space. Heavier loads result in more pain with irritation and effusion in the knee joint. There is also often local overheating of the knee joint.
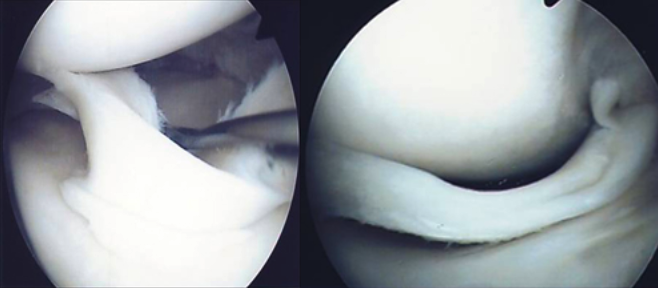
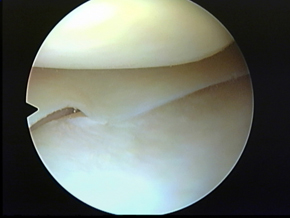
Fig.4: Unstable large basket handle tear (left) and blockage due to popped-out basket handle tear (right).
What exactly does the orthopedist examine?
The diagnosis can be made by a specific clinical examination in the area of the inner and outer meniscus. In addition, standardized X-ray images taken while the patient is standing. Also the exclude bony causes of the complaints and to determine the degree of arthrosis. Magnetic resonance imaging (MRI) is certainly the most reliable method to visualize a meniscus tear. From our point of view, an exact diagnosis of the meniscus injury is necessary to initiate the appropriate individual therapy.

Fig.6: MRI images of intact outer meniscus (left), intact inner meniscus (center) and meniscus tear (right).
Is it possible to avoid surgery?
If the patient is free of symptoms, a conservative (non-surgical) therapy can be attempted with physiotherapy and appropriate medication. Especially in older or less active patients, surgery can often be avoided.
When is an endoscopy (arthroscopy) necessary?
In most cases, however, there are persistent complaints in everyday life, which limit the quality of life significantly. It is then recommended to perform a knee arthroscopy. This allows excellent visualization and examination of the articular cartilage and menisci while treating the damage. Basically, it is important to preserve as much functional meniscal tissue as possible in order to reduce the long-term consequences of meniscal surgery. For this reason, preserving the meniscal tissue as much as possible by suturing it is absolutely necessary.
Tear in the meniscus – how to repair it?
We have a variety of different suture techniques and are very familiar with meniscus suturing. Only this allows for optimal fixation of the torn meniscus and creates optimal healing conditions.
Especially in the case of a basket handle tear, preservation of the meniscus is reasonable, since removal of the large basket handle flap would otherwise be equivalent to extensive meniscus removal.
What if the meniscus has to be (completely) removed?
Patients who lose their meniscus in an accident at a young age may develop early arthrosis in the medium term. This is often combined with the early onset of painful cartilage damage of the femoral condyle and the tibial plateau. Pain and bruising in the knee joint are the first signs of the development of arthrosis and an important indication of early overloading of the joint section.
What exactly is a meniscus transplant?
An important surgical procedure in this situation is the transplantation of a donor meniscus. Both the inner and outer meniscus can be replaced. The donor meniscus is ordered from internationally accredited tissue banks. It comes from deceased accident victims who had agreed to the removal. A rejection reaction is unusual.
The donor meniscus is removed under sterile surgical conditions and then tested under internationally accepted criteria for pathogens. The risk of transmission of an infectious disease is extremely low, but cannot be excluded. After appropriate storage and complex transport, the meniscus transplantation is performed minimally invasively during a joint endoscopy. The operation is complex and takes about 2 hours. We are very familiar with the technique of meniscus transplantation since more than 10 years and perform about 15-20 meniscus transplantations per year for private and health insurance patients. All meniscus transplantations are performed by Prof. Siebold.
What is the scientific status and what are the success rates?
Clinical studies show a significant reduction in pain and very good healing of the donor menisci, and most patients do very well with the donor meniscus. Long-term studies also show that the clinical success rate with good cartilage conditions is about 80%. Under certain conditions, additional operations for leg axis correction may be necessary in order to achieve optimal relief of the damaged joint section and the donor meniscus.
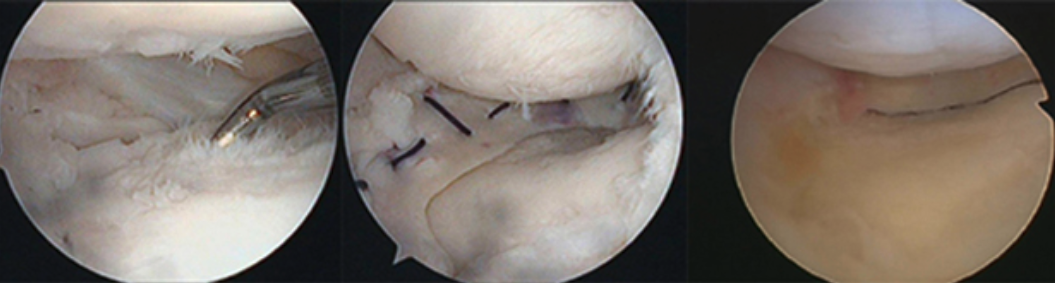
Fig.9 Cartilage damage without meniscus (left), donor meniscus after implantation (center) and healed donor meniscus (right).
Does it always have to be a donor meniscus? What about synthetic variants?
Because it is often very difficult to obtain a donor meniscus, intensive scientific work focuses on producing a synthetic implant to replace damaged meniscus tissue. The aim is to reduce pain and stimulate tissue growth in a damaged meniscus. The replacement tissue is sutured into the defect area of the inner or outer meniscus so that new, meniscus-like tissue forms and grows in. The implantation is minimally invasive, as a part of a knee joint endoscopy (arthroscopy). Currently, meniscus replacement implants are only suitable for a partial replacement of the meniscus and are not recommended for complete meniscus loss. Two different implants are available on the European market at the moment: „Actifit“ and „Menaflex“ (formerly: CMI – Collagen Meniscus Implant).
What happens after the surgery, how long does mobilization last?
After partial removal of the meniscus, full weight-bearing can already be performed on the day of surgery, with appropriate joke-oriented transition. One can use forearm walking sticks. Physiotherapy is recommended in the first weeks after the surgery. Office activities can be resumed after about 1 to 2 weeks. In the case of physical activity, it takes a few more weeks before the patient can return to active daily life.
And after the transplant/ graft?
After meniscus transplantation, the partial loading phase is extended to 5 to 6 weeks, otherwise there are no significant differences compared to meniscus suturing. After implantation of meniscus replacement tissue (e.g. ACTIfit), approx. 6 weeks of partial loading are necessary.
Which sports are possible?
After a partial meniscus removal, the knee can be carefully loaded without crutches already on the day of the operation. Cycling is possible after a few days if healing proceeds normally. Swimming follows about 3 weeks postoperatively after wound healing is complete. Jogging and stop-and-go sports (e.g. soccer) are not recommended until three to four weeks after surgery.
What about sports activity after a meniscus suture?
After meniscus suturing, sports rehabilitation can be delayed by several weeks. Here we recommend sports after 4-6 weeks at the earliest. Cycling and swimming are recommended. Movements like squatting should be avoided for at least 3 months to prevent bruising of the meniscal suture. Intensive sports should not be practiced in the 5-6 months after surgery.
And what about sports after a meniscus transplant?
After transplantation of a donor meniscus as well as implantation of meniscus replacement tissue, a return to light sports is possible after 5-6 months. Initially, we recommend cycling and swimming. The return to intensive sports must be carefully considered and is possible after 10-12 months at the earliest.
Through regular clinical checks and a slow build-up of the physical strain, a return to sports is possible in most cases. However, after meniscus transplantation ot the implantation of meniscus replacement tissue, competitive sports are only possible in exceptional cases.
Do you have any further questions?
Would you like to learn more or are you personally affected? Then contact Prof. Dr. Siebold directly. He will be glad to help you.
Cruciate ligament injuries - Anterior cruciate lugament (ACL)
What is the anterior cruciate ligament? And how does it get injured?
The knee joint is stabilized by the anterior and posterior cruciate ligaments. Especially sports accidents such as soccer or skiing, but also other twisting and falling injuries can result in a cruciate ligament rupture. It can lead to instability in the knee joint with unsteadiness („giving way“), pain and swelling. An untreated cruciate ligament tear often means the end of sports. Further damage to the meniscus and cartilage leads to painful swelling, to an irritable knee and finally to arthrosis. That is why „cruciate ligament replacement“ = „cruciate ligament plastic surgery“ is now standard in the treatment of cruciate ligament tears to restore knee function and protect the meniscus and cartilage.
Fig.1: Different parts of the anterior cruciate ligament (left), anatomical preparation of the anterior cruciate ligament (right).
Fig.2: Microscopic study of the anterior cruciate ligament, lateral section, ACL stained green on the left.
Which treatment is most useful for ligament rupture?
A suitable cruciate ligament replacement is crucial. Everyone from sports professionals to hobby athletes are treated with the individual surgical technique. The surgery preserves as much original cruciate ligament tissue as possible to improve proprioception and rapid healing. A partial tear of the anterior cruciate ligament is followed by a partial replacement of the anterior cruciate ligament (also called augmentation). Depending on the patient and sport, the semitendinosus tendon, patellar tendon or quadriceps tendon are used as grafts. A knee joint endoscopy requires only a few small incisions and is thus one of the gentlest procedures.
Fig.3: Autologous transplantation of the cruciate ligament, patellar tendon (left), quadriceps tendon (center) and semitendinosus tendon 3-4 fold (right).
What is special about double bundle reconstruction and flat cruciate ligament reconstruction?
Only since a few years it is known that the anterior cruciate ligament is flat instead of round. It ultimately looks like a wristband and is about twelve to 15 millimeters wide with a thickness of only three to four millimeters. Own anatomical studies could prove this. For this reason, a flat reconstruction of the cruciate ligament with the semitendinosus tendon (knee flexor tendon) using the double-bundle technique is an ideal option. A wide but flat reconstruction is created that closely resembles the anatomical shape of the cruciate ligament. This technique also has biomechanical advantages compared to the usual single-bundle technique. Therefore, we successfully use the double-bundle reconstruction of the ACL. Clinical follow-up examinations of patients show excellent knee stability with very high patient satisfaction.
Why choose the semitendinosus tendon as a replacement?
In 2018, we introduced a new surgical technique in which the semitendonous tendon is used as a flat cruciate ligament replacement. The new surgical method is innovative and very close to the natural cruciate ligament anatomy. It is the answer to the flat cruciate ligament anatomy and is a good alternative to the double bundle technique.
Fig.4: Anterior cruciate ligament replacement with autologous semitendinosus tendon using the double-bundle technique, arthroscopic (left) and MRI (right).
What is meant by a partial tear or partial rupture of the anterior cruciate ligament?
In the case of a partial tear of the anterior cruciate ligament, there is still rest stability in the knee joint. But sports that put a lot of pressure on the knee, such as soccer, handball, etc., with a lot of twisting and stop-and-go movements, can no longer be practiced. This is why partial reconstruction of the anterior cruciate ligament by surgery is useful in cases of instability, to strengthen the cruciate ligament. We use the double-bundle technique, keeping most of the cruciate ligament fibers that are still intact. The procedure is known as augmentation, and we are one of the few centers in the world that have used this technique for years. This provides the proprioception, the rest stability and the vascular supply of the original cruciate ligament and helps to achieve a rapid recovery.
When is the right time for surgery?
The right time is different for each patient. It depends on various factors. Ideally, there should be a good range of motion and low pain before surgery, because then the patient can rehabilitate quickly after the operation. The most feared complication after surgery of the anterior cruciate ligament is the postoperative reduction in flexion and extension (arthrofibrosis), which extends the rehabilitation period and often requires anesthesia mobilization or even further arthroscopic surgery. Considering the above criteria, the risk of arthrofibrosis is low.
Further reading: „Anterior Cruciate Ligament Reconstruction“ by Professor Siebold published by Springer.
Which graft is the right choice and what about returning to sports?
For young soccer players, professional soccer players and competitive athletes, we use the patellar tendon as a replacement. The patellar tendon graft grows in with its 2 bone blocks within 8 weeks and allows a early return to play after about 6-8 months possible. However, this is only possible with optimal daily rehabilitation of several hours(!) and professional athletes. The use of a patellar tendon can cause pain and numbness in the treated area below the kneecap. This is why tendon removal is not suitable in knee-active professions, such as tilers or kindergarten teachers.
A very good alternative to the patellar tendon is a knee flexor tendon = semitendinosus tendon. Today, we usually only remove the stronger semitendinosus tendon and spare the gracilis tendon. The removal of the knee flexor tendon usually does not cause any problems at the removal site and is very well tolerated. Also, the tendons can grow back within a year to a certain extent. With the semitendinosus tendon, we reconstruct the two parts of the anterior cruciate ligament using the so-called double bundle technique and can also perform a partial reconstruction (augmentation). This surgical technique is also ideal for competitive and ambitious athletes, because it restores the biomechanics very well and the durability is very good.
Depending on the sport and the patient, we also like to use the middle third of the quadriceps tendon. It is also an excellent graft but requires another skin incision above the patella. It is especially useful for patients who kneel a lot, whether at work or in sports.
Finally, we offer the possibility of using a donor tendon (allograft) for cruciate ligament replacement. This must be ordered from a tissue bank. Donor tendons are used especially in complicated revision surgeries and multiple ligament injuries.
And what to expect after the surgery?
We recommend an approx. 2-day stationary stay with medical supervision by our medical team for cruciate ligament replacement. Our experienced physiotherapists start rehabilitation already on the ward. Individual physiotherapy takes place twice a day and involves mobilization with walking exercises. Lymphatic drainage reduces soft tissue swelling. The offer of physiotherapy on Saturdays and Sundays is probably unique.
Do you have any other questions?n?
Would you like to learn more or are you personally affected? Then contact Prof. Dr. Siebold directly. He will be glad to help you.
Crutiatce ligament injuries - Posterior cruciate ligament
What are injuries to the posterior cruciate ligament?
Posterior cruciate ligament injury is much less common. It results in posterior knee joint instability. It is essential to initiate therapy immediately after the injury and often there are combination injuries with collateral ligament instabilities.
What are the acute injuries?
If the fresh tear of the posterior cruciate ligament is detected in the first days after the accident, a stable knee joint can be achieved in many cases by non-surgical therapy with a special splint. In order for the posterior cruciate ligament to heal, the special splint must be worn consistently day and night for 2-3 months.
In many cases, a fresh rupture of the posterior cruciate ligament can be treated non-operatively with a special orthosis to stabilize the knee joint. It must be worn consistently for two to three months. Alternatively, stabilization and healing of the torn parts of the ligament can be achieved in active, athletic people with a simple arthroscopic operation (so-called „augmentationplasty“). Fresh combined injuries with a tear of the posterior cruciate ligament and other ligament injuries should usually be stabilized surgically as early as possible.
What are chronic posterior cruciate ligament injuries?
Older posterior cruciate ligament injuries with little posterior instabilityIf there is a chronic injury of the posterior cruciate ligament with severe instability of the knee joint and significant functional problems, there is an indication for surgery. In these cases, cruciate ligament reconstruction is recommended, often requiring additional ligament replacement surgery of lateral ligaments. These combined operations are require a particularly high level of personal experience of the surgeon. What surgical technique is used?
As with anterior cruciate ligament reconstruction, the knee flexor tendons are usually used to replace the torn posterior cruciate ligament. Alternatively, a part of the quadriceps tendon from the femur can be used. The graft is inserted arthroscopically and stabilized. Additional tendon ruptures should also be treated. Cartilage or meniscus damage is additionally repaired at the same time.
What is the aftercare like?
The follow-up treatment is complex and must be carried out carefully. Partial weight bearing with walking sticks will be necessary for 6 weeks. The range of motion is also increased only slowly over this period, so that often a free range of motion in the knee can only be achieved after 2-3 months. After surgery, a special knee brace will be necessary, which is worn for about 3 months. A return to physical work or sports will be discussed in detail with the patient.
Do you have any other questions?n?
Would you like to learn more or are you personally affected? Then contact Prof. Dr. Siebold directly. He will be glad to help you.
Ligament instability
What exactly is knee instability?
Complex knee instabilities are instabilities of the knee joint in several directions, usually caused by correspondingly severe accidents (e.g., rupture of the anterior and posterior cruciate ligaments after knee rotation). For example, the absence of the anterior cruciate ligament causes anterior instability, the absence of the posterior cruciate ligament causes posterior instability, the absence of the medial ligament causes instability at the internal joint space, and so on. Thus, for each direction, there is one or more retaining structures. To treat such multidirectional instability, it is often necessary to repair (acute phase) or replace (chronic phase) several structures at the same time.
What examinations are made in the clinic?
In addition to the clinical examination, X-ray, MRI (magnetic resonance imaging) and sometimes also a computer tomography (CT) are necessary. Only then can surgical stabilization be tackled after precise therapy planning. For this purpose, depending on the injury pattern, different ligament reconstructions with different tendon grafts are performed, e.g. reconstruction of the anterior or posterior cruciate ligament or the lateral ligaments, etc. The surgery requires a lot of experience, with which we have in the area. Aftercare is also usually complex and requires patience in order to achieve good ligament healing.
Do you have any further questions?
Would you like to learn more or are directly affected? Then feel free to contact our experts Professor Siebold and Professor Becher. They will be glad to help you.
Disease of the patella (kneecap)
A large number of knee joint diseases affect the joint between the kneecap (patella) and the femoral condyle (femur), the so-called „patellofemoral joint“.
What are the reasons for pain in the kneecap?
Patellar complaints are often triggered by a bony congenital deformity of the patella or the sliding bearing. As a result of the deformity, a „misalignment“ of the patella develops with overpressure of the cartilage, pain, swelling and increasing cartilage damage. The patella can also slip out of the bony sliding bearing, which is called patellar dislocation or luxation. A (sports) accident can also lead to patellar luxation.
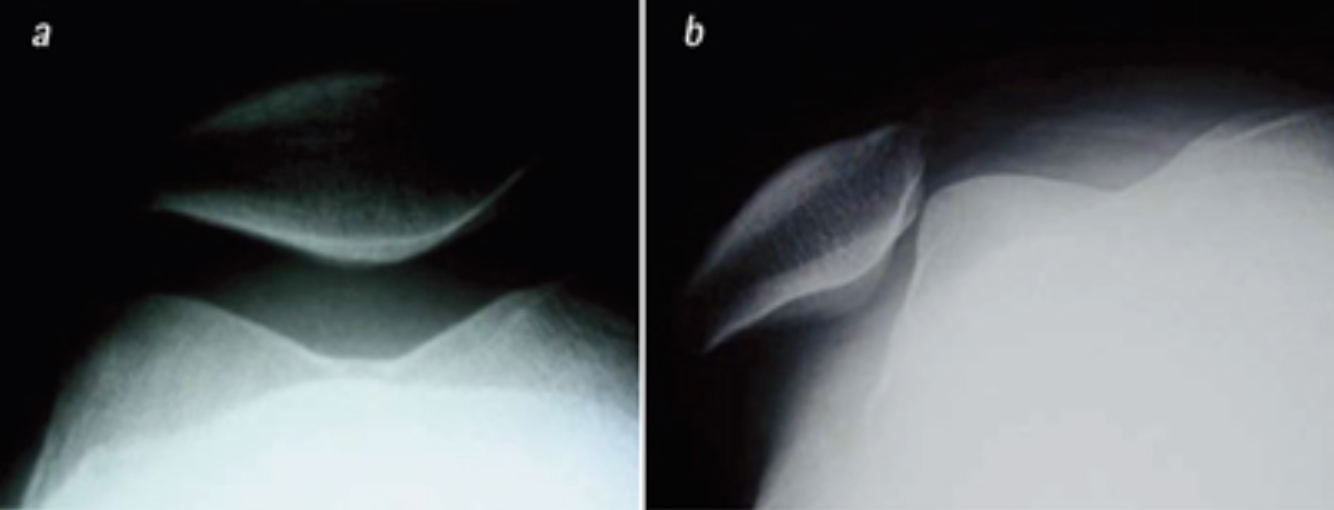
Fig.1: Centered (left) and externally „popping out“ (right) patella = lateral patellar luxation in x-ray image.
What is cartilage damage of the patella?
Malalignment of the kneecap or instability can cause pressure on the cartilage. Over time, this can result in cartilage damage developing behind the kneecap and in the femoral condyle, which can eventually lead to arthrosis. X-ray and magnetic resonance imaging precisely identify the cause. Furthermore, the severity of cartilage damage can be easily determined.
Does cartilage damage to the patella require surgery?
Not necessarily. Often, physiotherapeutic treatment can improve the symptoms and even eliminate the pain. Sports that reduce the strain on the kneecaps are cycling with a high frequency and less resistance (so-called spinning), crawl swimming, aqua jogging, paddling, Nordic walking etc.
The injection of hyaluronic acid preparations, which have a kind of lubricating effect, has proven more and more successful. It is also possible to inject „repair enzymes“ (ACP), which have a positive effect on cortex stabilization. Taking food supplements like glucosamine and chondroitin sulfate also has an effect.
And what is the surgical method for cartilage damage to the patella?
Arthroscopic cartilage cell transplantation is performed to repair deep cartilage holes. A detailed description of the different surgical cartilage therapy procedures can be found under the heading cartilage damage.

Fig.2: Spheroids for implantation in a cartilage defect (©Co.don)
Regarding the instability of the patella – how can it be treated conservatively?
When the patella is first dislocated, a ligament can tear (= medial patellofemoral ligament or abbreviated MPFL), which is crucial for the stable guidance of the patella. Conservative therapy without surgery involves strengthening the thigh muscle (M. quadrizeps) as well as coordination training by means of physiotherapy.
How to treat it surgically?
Indications for surgical intervention for patellar instability include: bony deformities of the patella or gliding bearing (also called dysplasia), recurrent instability, young active patients, cartilage damage, or torn free joint tissue.
When is a so-called MPFL used?
The medial patellofemoral ligament – or simply called MPFL – is a strong internal capsular reinforcement that runs from the edge of the patella to the femoral condyle. It stops the patella from popping outward from its sliding bearing during knee extension. Anatomical and biomechanical studies show the outstanding importance of the method as the most important stabilizer for the patella. The MPFL reconstruction has therefore proved to be very successful. The aim of MPFL reconstruction is to fix the patella back in the joint, repair any cartilage damage that has occurred in the process and limit further damage.
What is a MPFL surgical technique?
MPFL replacement has become the most modern and successful surgical procedure in recent years. In this procedure, the medial patellofemoral ligament (MPFL) is replaced by an autologous knee flexor tendon, the gracilis tendon. The tendon is inserted as a graft at the site of the torn MPFL and is secured by absorbable implants. The operation is a minimally invasive surgical technique.
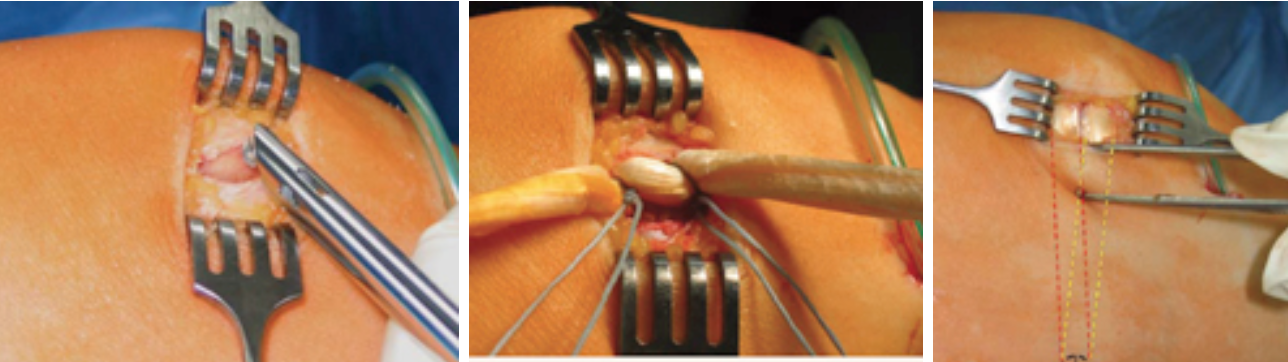
Fig.3.: Minimally invasive drilling of the bone tears at the medial condyle (left), fixation of the MPFL graft to the patella with special sutures (center), reconstructed MPFL graft at the patella with paralateral side course (right).
What is special about arthroscopic MPFL replacement?
Compared to the open technique, we perform MPFL replacement arthroscopically. We have developed our own surgical procedure for this. First, the MPFL is arthroscopically visualized on the patella and thigh. An exact understanding of the anatomical course of the MPFL is a necessary for this. With acute but also with recurrent patellar dislocation, the remains of the MPFL can be seen clearly as a broad but thin ligament. An arthroscopic replacement gracilis tendon is then pulled in and attached to the patella without implants and to the thigh with a bioscrew.
What are the main benefits?
Advantages of the arthroscopic approach are less trauma compared to the open approach, an individual anatomical reconstruction by exact arthroscopic visualization of the MPFL at the patella and femur, and a better aesthetic result due to smaller incisions at the patella. Recovery is easier due to less wound pain.
What rehabilitation measures does the patient face?
After surgery, pain-oriented range of motion can be increased to achieve free flexion after approximately 3-4 weeks. A motorized splint helps to speed up the rehabilitation process. In our opinion, partial weight-bearing is useful for about 2-3 weeks.
What are the scientific results on MPFL reconstruction?
Current studies on MPFL reconstruction show good to very good clinical results. The re-luxation rate is less than 4% (Christiansen et al 2008, Watanebe et al 2008, Mikashima et al 2006, Steiner et al 2006). This makes the surgical procedure very successful compared to other stabilizing procedures on the patella with reluxation rates of 10% -35% (Davis and Fithian 2002). The clinical and functional outcome, as measured by the Kujala score, is also convincing.
Do you have any further questions?
Would you like to learn more or are you directly affected? Then contact Prof. Siebold and Prof. Becher directly. They will be glad to help you.
Malpositions of the legs
What is meant by a malposition of the legs?
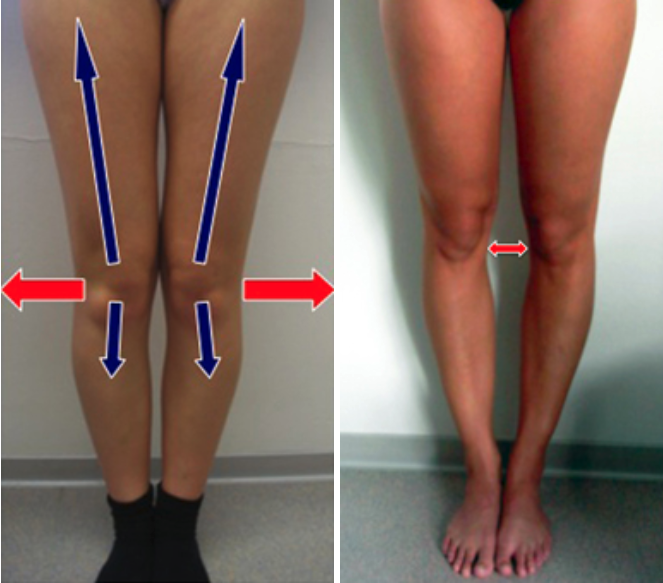
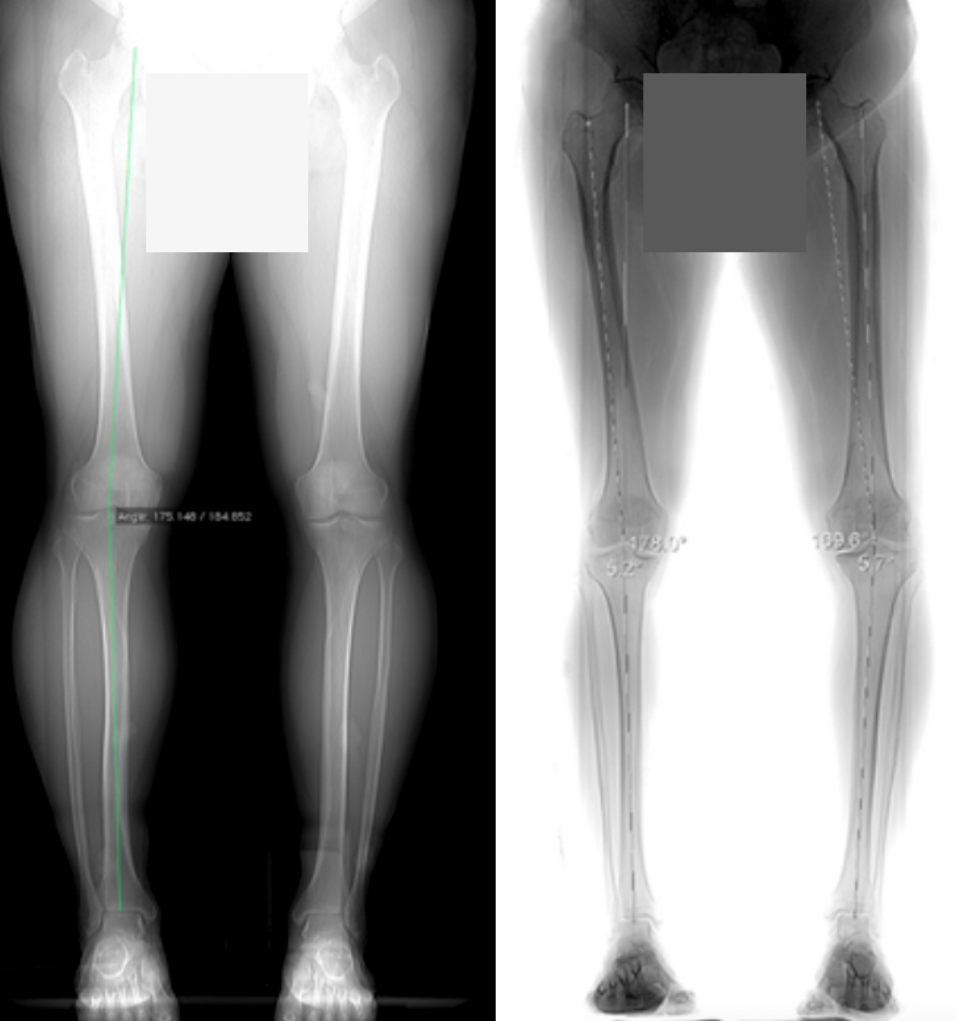
Leg axis malalignment is a deviation of the leg axis and joint surface angles from their normal measurements. Our anatomical axis between femur and tibia is normally about 7° valgus (=X-leg position) and the mechanical axis (so-called Miculicz line) between both bones is 180°. Both excessive genu varum (bow leg) and excessive genu valgum (X leg) can lead to overload symptoms, wear and tear and painful arthrosis over time. Therefore, it is important to treat them on time to reduce early damage. Leg axis correction can slow the progression of arthrosis and significantly reduce pain.
What are the differences?
Leg axis deformities are differentiated between congenital and acquired deformities. For example, a strongly hyperextended knee joint (genu recurvatum) is a congenital deformity. But an excessive bow leg (genu varum) or knock-kneed leg (genu valgum) is also often inherited on both legs. Inherited leg axis deformities can result from accidents, for example. Fractures, injuries to the growth plates in childhood and adolescence, or severe knee joint arthrosis can cause deformities of the bones and result in leg axis changes. Also, the reason for the leg axis malposition can be found in the area of the hip or foot. Less common causes are inflammations, bone metabolism disorders and systemic diseases.
What symptoms to look out for?
Malpositions of the leg axis have an unfortunate effect on the distribution of pressure in the knee joint. The result is a one-sided load and irregular abrasion on the inside or outside of the joint. This can lead to symptoms of overloading at the age of 30 to 40, causing pain on exertion and at rest. Painful bone edema, degenerative meniscus lesion, cartilage abrasion, joint space narrowing and finally unilateral knee joint arthrosis occur. It can also lead to functional limitation of the knee joint. The symptoms develop insidiously. One should also take a closer look at the family history. External influences, such as a sports accident, can greatly increase the natural (often gradual) progression of the disease. Causes are particularly injuries to the meniscus and cartilage. Ligament instabilities (e.g. anterior cruciate ligament damage) may also significantly increase the incorrect loading in the case of leg axis malalignment.
Why is it important to pay attention to the individual leg axis when treating acute or chronic joint damage?
Quite often, an injury to the inner meniscus or the cartilage on the inside is associated with genu varum (bow leg). The reverse case, i.e. injury to the outer meniscus or cartilage on the outer side with genu valgum (knock knees) is also quite common. In both cases, it is necessary to treat them carefully. Under certain circumstances, it makes sense to combine arthroscopic joint surgery to repair the meniscus and cartilage damage with corrective leg axis adjustment to ensure the success of the treatment.
Fig.2: X-ray while standing, inner joint space significantly reduced due to wear of the meniscus and cartilage.
How do the diagnostics look like in this case?
During the clinical examination, the leg axis is first examined in the standing position. Precise measuring of the angles between the femur and tibia is possible by radiological whole-leg imaging of the long tubular bones. Today, the anatomical leg axis is measured digitally. In addition, X-rays should always be taken while the patient is standing under body weight load (Rosenberg View and a sagittal image) to determine the (residual) width of the joint space. Only in this way is it possible to plan a meaningful therapy.
What is the conservative treatment for leg axis malalignment?
The aim of treating malalignments of the leg axis is to relieve pain, improve patient’s life quality and normalize mobility as far as possible. Joint wear and tear should be prevented and the development of arthrosis delayed. It is important to explain the consequences of joint malpositions on the formation of joint wear to the patient. It is also important to communicate the influence of conservative and surgical therapy on the progression of arthrosis.
What is better not to do in case of malposition?
In acute pain phases, we advise avoiding overloading the knee joint by engaging in more vigorous sports, e.g., stop-and-go sports such as soccer, squash, etc. Reducing weight is also often very helpful. Load must be adjusted to reduce symptoms. Specific physiotherapy, pain medication and shoe adjustments also provide relief.
What other conservative measures are available?
Hyaluronic acid preparations have also been successfully used in this case. Nevertheless, a surgical correction of the leg axis should be considered at the beginning of the symptoms, especially in the case of severe leg axis deviations and young patients. This is the only way to correct the load axis and prevent early wear and tear of the joint. The correction should be done at a time the meniscus and cartilage are still intact.
What is the surgical therapy for leg axis malpositions?
In the case of severe complaints in everyday life, sports and work, surgical therapy is usually necessary. The condition that pain is present and comprehensible by radiological imaging and that there is a prospect of improvement by leg axis correction. The correct indication is crucial in order to achieve the highest possible success rate through surgery.
What role does the patient play in successful therapy?
Age, weight, knee joint mobility, ligament stability, extent of leg axis deviation, concomitant damage to the joint, the patient’s activity level and the job play an important role. The patient’s compliance must also be considered. This is because follow-up treatment requires patience. The patient’s expectations with regard to realistic ( sports-related) stress are very important. It must be made clear to the patient that a leg axis correction cannot cure arthrosis. But ideally it reduces the symptoms for a long time. Nevertheless, sports load after a leg axis correction must be performed carefully. Another goal of surgery is to delay artificial joint replacement as long as possible.
How does the surgical correction of bow-leg deformities look specifically?
There are two correction options for bow-leg malalignment (genu varum). The most common is the open wedge- Osteotomy with internal opening of the tibial head and fixation with an angle-stable plate directly below the knee joint. Depending on the extent of the correction, it may be necessary to fill the resulting gap with bone that can be obtained from the iliac crest. More rarely, the „closed wedge osteotomy“ is performed. In this procedure, a wedge of bone is removed from the external tibial plateau below the knee joint, resulting in the required genu valgum (x-leg) after closing this wedge-shaped gap and fixation with an angle-stable osteosynthesis plate.
Fig.4: Open wegde osteotomy using angle-stable TomoFix plate, during surgery (left) and 6 months postoperatively (right).
How is the surgical correction of x-leg deformities performed?
Excessive x-leg deformity (genu valgum) is less common and is treated surgically on a similar principle. Usually, the bony deformity is not located at the tibial plateau but in the area of the femur near the knee joint. After radiological confirmation, a varus leg axis alignment is made on the femur directly above the knee joint. The operation is much more difficult and the healing process takes longer. Rarely, in the case of minor corrections, a narrow bone wedge can also be removed from the inside of the tibial head and, after closing the gap, fixation with an angle-stable plate can be performed here.
Why do X-rays during the surgical procedure?
The individual surgical steps are closely monitored and documented by intraoperative X-rays. During surgery, the extent of the leg axis realignment is also checked. Postoperative radiographs after about 4 to 6 weeks show the healing process and the consolidation of the osteotomy gap. The osteosynthesis plate should be removed with the screws after about 6 to 12 months.
What do the aftercare treatments look like?
Today, we exclusively use a modern and particularly angular stable plate system (Tomofix), which was developed only a few years ago. With this system, the patient can, in most cases, resume full weight-bearing after only 2 to 3 weeks and dispense with walking aids after 6 weeks. The inpatient stay is about 4 to 5 days. Early functional physiotherapy accelerates the healing process and should be performed 2 to 3 times per week. Stand-up cycling and water gymnastics (crawl swimming, aqua jogging) are also useful after the wound has healed from the 3rd to 4th week.
What are the prognoses?
The natural progression of a leg axis deformity cannot be accurately predicted individually. A scientific prognosis of the correlation between gonarthrosis and leg axis deformity is not possible. Nevertheless, it can be stated that 10 years after surgical leg axis correction, 75% of patients still have not received a knee joint prosthesis.
Knee injuries and diseases in children and adolescents
Cartilage damage in children and adolescents
Do cartilage injuries occur in children and adolescents?
Cartialge lesions in kids and adolescents are usually caused by a sports accident. We specialize in the complete repair of cartilage holes by minimally invasive arthroscopic cartilage cell transplantation. We perform about 100 cartilage cell transplants per year in children, adolescents and adults. A special form of juvenile cartilage damage is the so-called „osteochondrosis dissecans“ (OD), which occurs in different stages and can lead to pain and large cartilage-bone defects in the knee joint.
Do you have any further questions?
Would you like to learn more or are directly affected? Then feel free to contact our experts Professor Siebold and Professor Becher. They will be glad to help you.
Crutiate ligament injuries in children and adolescents
Can children and adolescents have an ACL injury?
Injuries to the anterior cruciate ligament are also common in children and adolescents, particularly as a result of sports.
There are two main types of cruciate ligament injuries in children: On the one hand, there may be a direct tear of the cruciate ligament fibers in the joint and on the other hand – and this is typical for children – there may be a rupture of the anterior cruciate ligament on the tibia. In both cases, the knee joint is unstable. Through a precise clinical examination compared to the healthy side and according to x-rays and magnetic resonance images, the expert physician can make a definite diagnosis.
What is the cruciate ligament replacement and how can it be treated?
Based on clinical experience, early recovery of stability is necessary to avoid damage to the cartilage and menisci at an early stage. Unfortunately, stabilization by muscle training alone is usually not sufficient. Only ACL surgery can restore the functionality of the knee joint and protect the knee joint from early wear and tear and arthrosis. Therefore, a pediatric cruciate ligament injury in children and adolescents should be treated surgically in case of instability of the knee joint.
What is so special about childhood and adolescence?
The specific things in children and adolescents are the open growth plates. If there is a bony avulsion of the anterior cruciate ligament on the tibia, the avulsed bone fragment should be reattached in an arthroscopic minimally invasive operation. This can be achieved very well without implants by using sutures. If the cruciate ligament is ruptured in the joint, a cruciate ligament replacement is recommended. For this purpose, we use the semitendinosus and gracilis tendon, which is pulled into the joint along the course of the original cruciate ligament tendons. Since the surgical technique requires the creation of drill channels on the tibial plateau and femur, it is important to treat the growth plates carefully. As long as important surgical rules are followed, no growth disturbance is expected. A novel surgical technique developed by Prof. Siebold for children and adolescents has significantly improved the durability of cruciate ligament reconstruction.
Do you have any further questions?
Would you like to learn more or are you personally affected? Then contact Prof. Dr. Siebold directly. He will be glad to help you.
Meniscus injuries in children and adolescents
When do meniscal injuries happen in childhood and adolescence?
An meniscus injury often occurs in sports or in accidents. The young patient can usually describe a corresponding event. Wearing of the meniscus without a corresponding trauma almost does not occur at this age.
What is the clinical examination looks like?
If these symptoms occur when a meniscus injury is suspected, an experienced pediatrician or knee specialist should be consulted to do further diagnostics. Usually, the symptoms can be confirmed by physical examinations.
In addition to the classic meniscus tests, it is also important to check the stability of the cruciate ligaments and the lateral ligaments. A possible popping out of the kneecap (patellar luxation) must also be examined.
Why is meniscus repair by suturing necessary?
Especially in childhood and adolescence, the suture of the meniscus is absolutely necessary to preserve the meniscus as a shock absorber and to protect it from arthrosis. Since the meniscal tissue has a great healing potential at this age, meniscal suturing is recommended.
(Special case) disc meniscus
The disc meniscus occurs as a rare variant of the outer meniscus. The meniscus does not have the typical shape of a sickle, but looks like a complete half-moon disc. Pain may be present on the outside of the knee joint. This form is prone to wear and tear in adolescence. Through our decades of clinical experience, we have a great routine in the treatment of the disc meniscus.
Do you have any further questions?
Would you like to learn more or are you personally affected? Then contact Prof. Dr. Siebold directly. He will be glad to help you.
Patella luxation in children and adolescents
What happens if the patella slides out of the plain bearing?
Auch im Kindes- und Jugendalter kann es zum Herausspringen der Kniescheibe aus dem Gleitlager kommen. Dabei kann eine bleibende Instabilität der Kniescheibe verbleiben, die immer wieder zum Herausspringen, Schmerzen und Schwellung führen kann. Neben starker funktioneller Einschränkungen können bleibende Knorpelschäden resultieren. Leider treten die Probleme nicht selten beidseits auf, insbesondere wenn die knöcherne Führung der Kniescheibe ungünstig ist. Deshalb ist eine genaue Diagnostik mit Untersuchung und MRT (Kernspin) wichtig, um einen genauen Therapieplan aufzustellen. Je nach Schweregrad kann ohne Operation mit Physiotherapie behandelt werden oder es muss eine operative Stabilisierung der Kniescheibe durchgeführt werden.
Do you have any further questions?
Would you like to learn more or are you personally affected? Then contact Prof. Dr. Siebold directly. He will be glad to help you.
Further therapy options
Conservative therapy
Shortly you will learn more about it here
Endoprosthetics
In principle, our goal is always to preserve the natural knee joint. Nevertheless, it may well make sense to replace all or part of the damaged joint. Reasons for this can be: Age (wear and tear), (rheumatoid) arthritis, (incorrect) stress, diet, body weight, metabolic diseases, accidents and injuries.
As the knee is a very complex joint, there are also different types of implants. There is a distinction between coupled, partially coupled and uncoupled prostheses for knee joint implants. This variety allows treatment measures with the principle: „As much as possible, not more than necessary.“
During an examination, we will clarify which treatment is right for you individually and whether a prosthesis is necessary at all. We will explain the alternatives as well as the opportunities and risks of the different procedures.
What is a total knee replacement (TKR)?
A total knee replacement or so called knee arthroplasty is a complete replacement of the knee joint with sparing removal of bone from the upper and lower leg. This type of prosthesis is used when both the inside and outside part of the knee joint are severely destroyed by arthrosis. In this case, a slide prosthesis (partial replacement) cannot help anymore.
The two joint components(of the upper and lower leg) are completely „crowned“ by the total endoprosthesis. The aim is a largely normal and pain-free knee function without pain from arthrosis.
The materials used are inert metal alloys, titanium as well as polyethylene (synthetic material). A rejection is nearly impossible. The main problem is the abrasion of the polyaethylene plate. This is mainly due to stretching and twisting movements in everyday life. Malposition of the leg axis causes significant unilateral wear and loosening of the surface replacement, producing renewed pain and dysfunction. However, a complete knee replacement can function very well for 10-20 years in most cases without the need to change the prosthesis.
What are the differences between a total knee replacement and a partial joint replacement?
In the case of advanced arthrosis, the only option is often to replace the joint with an implant. Two types of knee replacement are available: total knee arthroplasty (also known as TEP, which replaces the entire joint) and partial knee arthroplasty or partial joint replacement.
The best option depends on various factors and should be discussed individually with the specialist. Important for the successful treatment of knee joint arthrosis are detailed diagnostics and an individual therapy suitable for the patient.
There are many reasons why patients are more satisfied with a partial joint replacement: It preserves the natural joint function as long as possible. In addition, the operation is minimally invasive, less soft tissue is being destroyed, patients feel less pain and recover more quickly. One type of partial knee joint replacement is the sled prosthesis. In scientific terms, it is also called unicondylar tibiofemoral arthroplasty.
What is a sled prosthesis?
The sled prosthesis (unicondylar joint replacement) is a partial replacement of the knee joint. The surface of the affected joint section is crowned by the prosthesis. The surgery is minimally invasive and the implants are cemented in place, so the patient is usually mobile again after a few days. Activities such as cycling, swimming or hiking are already possible after a few months.

Fig. 3: X-ray images of knee joint preop (left) and postop with sled prosthesis (right)

Fig. 4: X-ray images of the sagittal knee joint preop (left) and postop with sled prosthesis (right)
What are the surgical options?
During the operation, the two worn joint components on the upper and lower leg are „crowned over“, similar to a dental implant. Because the surgery is performed by a minimally invasive approach, the patient is able to return to mobility after only a few days. It is allowed to put full weight on the operated leg immediately after the operation.
Various implants are available according to the size, weight and activity level of the patient. The advantage of all procedures is a low bone loss, which makes it usually much easier to change the prosthesis when it wears out, than to replace a complete prosthesis.
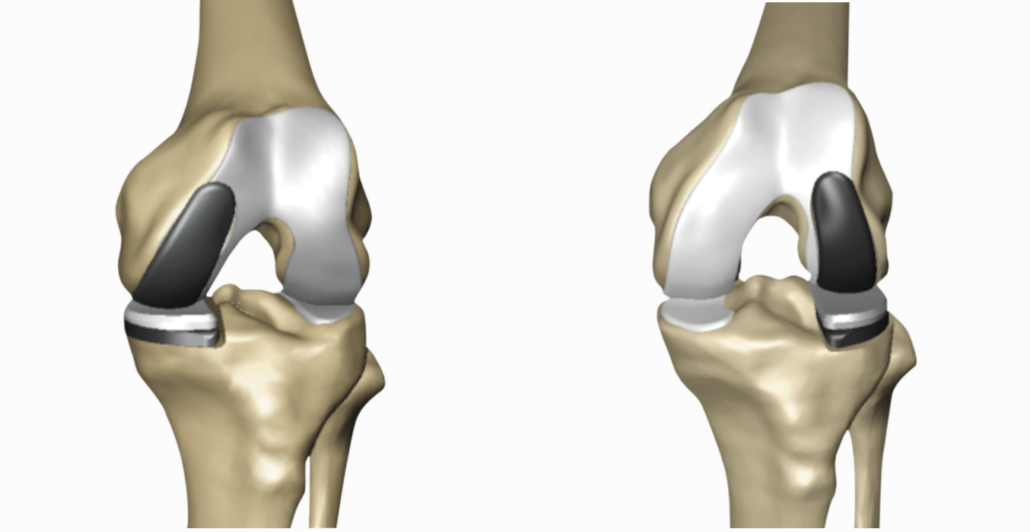
Fig. 5: Insertion of sled prosthesis laterally (left) and medially (right) with MAKO Smartrobotics®
What are the requirements for implantation of a sled prosthesis?
An intact anterior cruciate ligament as well as intact cartilage and meniscus in the area of the non-damaged part of the joint are required for the implantation of a sled prosthesis. It is not considered in cases of severe movement restrictions as well as severe leg axis deviations ( O legs or X legs).
We can look back on more than 20 successful years in the implantation of the sledge prosthesis. The operation is performed a few times a week by our experienced knee specialists.
MAKO robotics
What is MAKO Robotics?
„Accurate to the millimeter“ – this is important, especially in joint surgery, when operations have to be performed on delicate parts such as the hip or knee joint. Surgery on such complex joint structures, where bones lie close to tendons, ligaments and nerves, requires absolute precision. That is why we rely on the support of state-of-the-art technology in knee surgery. One of the most advanced is the so-called Mako SmartRoboticsTM®. More information on the methodology and advantages can be found on this page.
AMIC procedure for cartilage damage
What is AMIC® and when is this procedure used in knee surgery?
AMIC® stands for Autologous Matrix Induced Chondrogenesis and is mainly used to treat knee cartilage damage. It is a biological surgical method that has been successfully proven since 2003 for the treatment of damaged articular cartilage. It is called biological because AMIC® activates the patient’s self-healing process. The procedure is a development of microfracturing – in which an abrasio (freshening) of the exposed bone (subchondral bone plate) is made. As a result, blood and stem cells from the bone marrow come out and fill the damaged cartilage area. The blood clot contains all the necessary components for cartilage repair tissue formation. A matrix (a cut-to-size cartilage tissue called Chondro-Gide®) is then placed on top of the cartilage using fibrin glue for fixation and stabilization. The transferred cells settle in this matrix and can grow into cartilage-like tissue. In contrast to microfracturing, the method is also suitable for larger cartilage defects.
What else does the AMIC procedure do?
The AMIC® surgical procedure not only reduces pain, but also restores joint function over a wide area. The goal is to establish complete mobilization and return to the usual active daily life. The AMIC® procedure also slows joint cartilage degeneration, delays total joint replacement, or may prevent the need for knee arthroplasty.
What exactly is done during the surgical procedure?
First, a joint endoscopy (arthroscopy) is required to determine the level of defect damage and to remove any degenerative cartilage tissue. Using a sterile template, a mould of the defective cartilage is made and afterwards transferred to the Chondro-Gide® matrix. In the next step, an abrasion of the exposed bone is performed. The matrix is finally fixed to the defect area.
And after the operation? When is the patient ready to return to work?
During the first week, the patient should wear an orthosis for mobilization. Loading needs to be minimal and with crutches. In the following 2-6 weeks, the patient can switch to a motorized mobile splint with increasing range of motion. Free mobility is possible after six weeks. Full weight bearing is possible after 6 weeks if the patient is free of pain.
What scientific results can already be seen in clinical research?
The AMIC® procedure has proven itself over the years as an effective surgical method for cartilage repair in the knee joint, as confirmed by clinical studies. Of course, the results after repair of knee cartilage defects depend on the location and size of the joint defect, the age of the patient and any other defects in the knee joint. In some study, good results were observed especially with arthroscopic and minimally invasive procedures.
Change of a prosthesis (revision)
When does a replacement of the prosthesis be necessary?
In the case of loosening of a surface replacement, but also sometimes in the case of substantial loss after sled prostheses (especially older designs), it is necessary to correct the bone defect and to fix the prosthesis more firmly than during initial implantation.
For the repair of defect situations, corticospongiosal chips and blocks from the iliac crest or the bone bank (donor bone) as well as metal blocks are used in the area of the femur. As these bone plates must first grow in, the anchoring of the surface replacement naturally requires reinforcement of the basis with shafts of different lengths and sizes of the femur bone in order to correct the defect. Also in this case, the foundation of this prosthesis must be strengthened by inserting a stem into the lower leg bone for stabilization.
In addition, when prostheses loosen or the polyaethylene wears out, ligament instability often occurs, which requires stronger guidance. Prostheses of the newest design show still a slight rotational component of the posterior stabilization, therefore abrasion is also avoided in rotational movements the knee performs. Furthermore, there are also so-called „hyperflex“ polyaethylene inserts, which allow full flexion.
When is arthroplasty necessary and what are the benefits?
Endoprosthetics is necessary in the case of the most severe defect situation after repeated revision, but also after severe infections or loss of substance due to the strongest polyaethylene abrasion in the area of the bone bearing, as well as the most severe instabilities. Here, arthroplasty can lead more strongly and help compensate for the weakness of the ligamentous apparatus.
In terms of mechanics, the implants still resemble the origins of development, when there were coupled prostheses. This makes it possible to stabilize a complete thinning after the most severe malpositions. One of the disadvantages of simple hinged joints is, the enormous force of the shafts in the bones, which leads to loosening, especially in rotational movements, which can be corrected in a simple sagittal hinge. or this reason, in the development of modern coupled prostheses, rotation has been included, so that implanted prostheses in our clinic have a coupled rotational prosthesis design, which provide excellent functional results with excellent durability.
Do you have any further questions?
Would you like to learn more or are directly affected? Then feel free to contact our experts Professor Siebold, Professor Becher and Professor Thorey. They will be glad to help you.