Treatment of the hip joint
he International Center for Orthopedics specializes in the treatment of the hip joint. The hip connects the pelvis and the thigh. Since the hip is a ball and socket joint, the legs can be moved very flexibly in all directions.
Learn how a hip injury and hip disease manifests itself by clicking on the different sections. What symptoms should one pay attention to and when is it the best time to go to a specialist? You can also find out what treatment options are available today and what rehabilitation might look like after the surgery.
Hip injuries and diseases
Coxarthrosis (wear and tear of the hip joint)
What is coxarthrosis exactly?
Coxarthrosis is the gradual degeneration of the joint cartilage (wear and tear of the joint). The joint cartilage becomes cracked and loses substance. Since it is a gradual process over the years, coxarthrosis is not recognized immediately. Only over the years, when the arthrosis is already advanced, pain and movement restrictions appear.
What symptoms to look out for?
Arthrosis in the hip is often noticed by pain after prolonged sitting or lying down. These typical start-up difficulties are also followed by pain after prolonged exertion. In addition, the leg can no longer be spread or rotated properly. Muscle tension is also a clear sign of coxarthrosis due to the damaged capsule-ligament apparatus.
Most of those affected are already 50 years and older. Physical stress is often the cause of joint wear, but accidents or malformations (dysplasia) are also causes.
How can arthrosis in the hip be clinically diagnosed?
With the help of mobility tests, examination of the gait pattern, posture and palpation, the hip expert already obtains important findings. State-of-the-art imaging such as X-rays also provide information on the condition of the cartilage. MRI provides further details on soft tissue, ligaments and tendons. In this way, other diseases can be ruled out or fluid deposits can be identified.
Can coxarthrosis be treated conservatively?
With initial arthrosis, much can be managed by changing one’s lifestyle. A healthier diet, more exercise and weight reduction can reduce the risk of arthrosis.
Conservative therapies include pain and anti-inflammatory medications, physical therapy (muscle building), and injection therapy.
When is surgery recommended and what treatment options are available?
If coxarthrosis is already advanced, i.e., if the cartilage is already massively damaged, often only surgical interventions can help. Using hip arthroscopy, the joint cartilage can be examined directly. In this way, it is possible to determine whether a cartilage graft is necessary, a correction of malpositions (osteotomy) or a joint replacement.
Of course, joint-preserving measures are preferred. Which is the best therapy must be examined in each individual case and discussed with the patient.
Labrum damage
What is special about the hip joint and what happens when it malfunctions?
The hip joint is a ball-and-socket joint that runs along the acetabulum, allowing full movement in all three directions. Disorders of the hip joint can be caused by either a misalignment of the femoral head or the acetabulum, and are often manifested by load-dependent pain.
In both cases, a mechanical problem occurs when the head-neck transition of the femoral neck strikes the anterior glenoid cup, which can damage both the labrum and the articular cartilage, often leading to joint arthrosis.
Why is a comprehensive examination by a specialist so important?
As well as wear and tear of the hip joint (osteoarthritis), other damage and conditions close to the joint need to be looked at. It is not uncommon to find damage to the labrum.
What is the function of the labrum?
The labrum surrounds the hip joint and protects the free cartilage edge of the hip joint. This allows the joint surface to be enlarged and keeps the fluid film (synovia) in the joint space. As a result, low-friction movement is possible and wear on the joint is delayed. If the labrum is damaged due to misalignment, it will tear, similar to the meniscus tear in the knee joint.
Why should groin pain (when sitting) be taken seriously?
Pain in the groin is caused by the nerve supply to the labrum during stress or certain movements. The labrum becomes irritated. As most labral tears are in the anterior (front) region of the hip socket (62-92%), this is indicated by groin pain when sitting during daily activities.
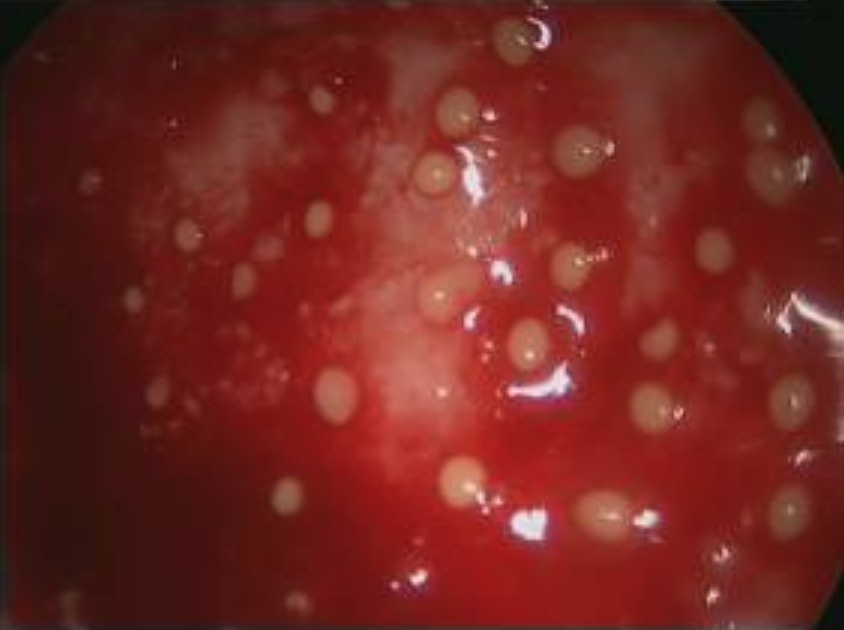
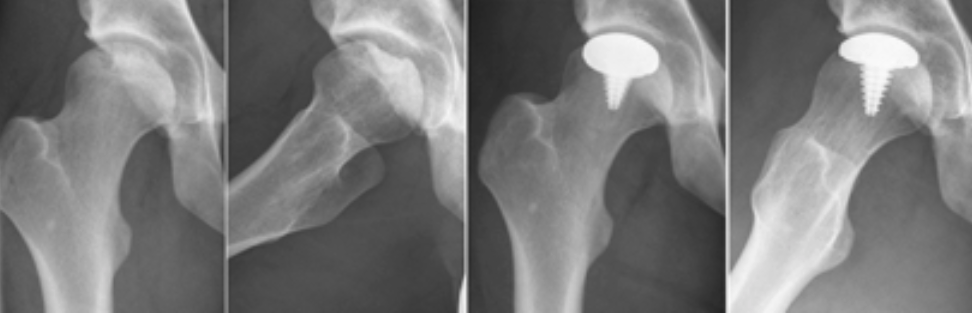
Figure 1: Degenerative labral tear of the anterior acetabulum (left), labrum detached from the acetabulum (right).
When this pain occurs, there is often a mechanical problem. In addition to the damage to the labrum, the articular cartilage becomes detached and exposed. The increased shearing forces on the cartilage can cause further damage, leading to osteoarthritis of the hip joint.
Figure 2: Loosened articular cartilage from the acetabulum in a severe labral defect with cam impingement.
What tests are performed in the clinic?
If labral damage is suspected, a magnetic resonance imaging (MRI) scan of the affected hip joint should be performed during the clinical examination. This involves injecting a contrast agent into the hip joint (MR arthrography). This method has a much higher sensitivity (92%) than standard MRI (62%).
Conservative or surgical? Why is surgery recommended?
Conservative treatment of labral tears is usually unsuccessful. Surgery can be performed by arthroscopy without causing major deformity of the hip joint. The damage is repaired through two to four small skin incisions using small instruments. Depending on the size of the defect and the nature of the labrum, the procedure may involve smoothing with removal of degenerative parts of the labrum or reconstruction with suturing of the labrum.
How much time will I spend in hospital and when will I be able to get back to work?
Follow-up treatment after arthroscopy of the labrum depends on the initial damage and the surgical treatment given. However, in many cases the patient will be able to do pain management and physiotherapy exercises on the first day after surgery. If additional work was done on the joint cartilage or bony structures during surgery, partial weight bearing is often required. Aftercare always depends on the individual case.
What are the scientific results?
The results of clinical studies show that arthroscopic treatment of isolated labral tears results in significant improvement in a large number of cases. Byrd et al showed that 83% of patients had good to excellent results. Similar results were found by Streich et al, Nepple et al, Yamamoto et al in their patient populations where they treated labral tears arthroscopically.
As a result, arthroscopic treatment of labral damage in the hip joint is now the first choice and offers patients a very good chance of improvement.
Hip impingement (FAI)
What is Femoroacetabular Impingement (FAI)?
Femoroacetabular impingement (FAI) is a condition of the hip joint in which pain is caused by the femoral neck hitting the acetabulum. Bony abnormalities are often found at the transition from the femoral head to the femoral neck (cam impingement) or at the acetabulum (pincer impingement).
What are the causes?
Cam impingement can be caused by a bump at the head-femoral neck junction, or by poorly healed conditions in childhood or adolescence (e.g. Perthes‘ disease, epipyseolysis capitis femoris). Causes of pincer impingement may be congenital (e.g. retroversion of the acetabulum, protrusio acetabuli) or acquired (e.g. degenerative attachments).
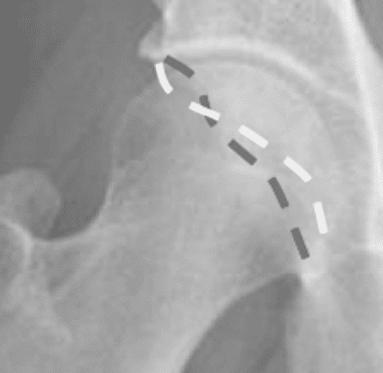
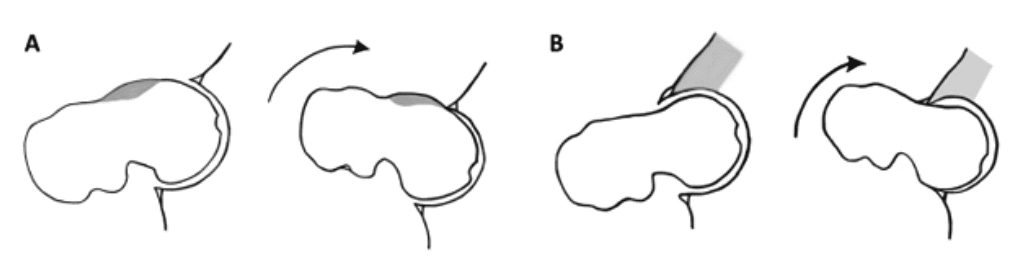
Fig.2: A typical pincer impingement with retroversion of the acetabulum (white=anterior acetabular cup, gray= posterior acetabular cup).
What exactly is so critical about it?
In both cases, mechanical problems are caused by the head-neck transition of the femoral neck striking the anterior glenoid cup, which can then damage both the labrum and, in time, the articular cartilage. In many cases, this leads to early joint osteoarthritis.
Fig.3: Cam impingement (A) or pincer impingement (B) causes the femoral neck to hit the acetabular cup.
What exactly does hip impingement feel like?
Patients often report pain in the groin, which can occur with prolonged sitting or during sports (e.g. hurdling, volleyball). Classically, the bony pathology does not improve with conservative treatment, so patients often report frustrating physiotherapy sessions.
How is FAI diagnosed?
The diagnosis of femoroacetabular impingement (FAI) is based on clinical and other diagnostic findings.
It is noticeable that the patient experiences increased pain, especially when the hip joint is flexed with simultaneous internal rotation and spreading of the leg (anterior impingement test). In this test, the head-femoral neck junction is pressed against the anterior acetabulum. If the hip is misaligned, full and smooth movement of the hip joint is not possible. This test can also provide information about possible damage to the labrum.
How do imaging techniques help?
X-rays of the affected joint provide information about bony deformities. Magnetic resonance imaging (MRI) with injection of a contrast agent into the joint (MR arthrography) is also an important additional test that can detect other pathology and possible sequelae before surgery, allowing the surgical procedure to be planned accurately.
How to operate a FAI?
Femoroacetabular impingement (FAI) is most commonly treated by arthroscopic surgery. Through 2-4 small skin incisions, special instruments are used to remove the bony attachments so that the hip joint can continue to move fully in all three directions without mechanical problems and pain.
When is minimally invasive surgery recommended?
More extensive, dorsally extending bony pathology sometimes requires a minimally invasive open approach (MIS, keyhole surgery), as some pathology is very difficult to treat using an arthroscopic approach.
How many days will I spend in hospital?
The length of stay in hospital depends on the type of surgery and can vary from three to seven days. Mobilisation and activity will also depend on the procedure and extent of the surgery, so each patient will receive an individualised physiotherapy and exercise programme for further outpatient treatment.
Cartilage damage
How do you notice cartilage damage in the hip?
The quality of the articular cartilage in the hip joint deteriorates after a few years due to degenerative processes. The early symptoms are load-dependent pain, which occurs mainly after prolonged stress.
What clinical examinations are carried out?
The medical history and clinical examination are supported by diagnostic imaging using X-rays and MRI.
Does hip cartilage damage require surgery?
There are many conservative treatment options available at this stage, including dietary management, specific exercise and specific medical treatments.
When does cartilage damage require surgery?
If the pain becomes severe and affects the individual’s quality of life (pain at rest, pain at night, etc.), further surgical treatment is recommended.
What are the treatment options?
Depending on the type of cartilage damage, there are different surgical treatment options. For deep defects involving the articular cartilage on the side of the hip socket or femoral head, microfracture is often used to remove the damaged cartilage and expose the underlying bone. The bleeding from the bone, including stem cells, then gradually forms replacement cartilage in the affected area, allowing normal use of the joint. In many cases, microfracture involves covering the defects with a collagen membrane (AMIC, Matrix Associated Chondroneogenesis) so that the migrated blood cells and stem cells remain in place.
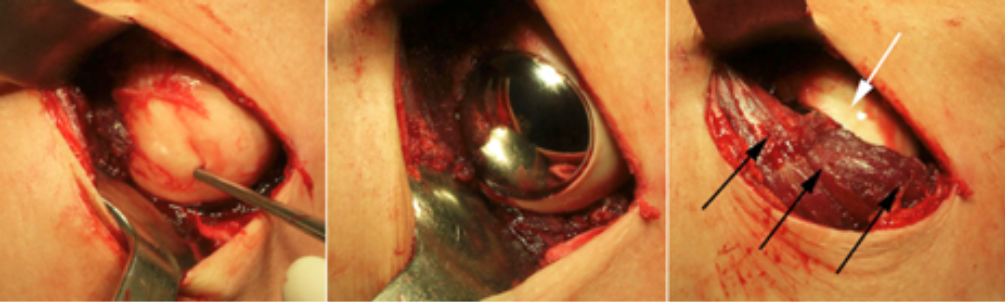
Fig.1: AMIC treatment of a cartilage defect on the acetabulum (*ChondroGide lying on top of the defect).
What exactly is autologous chondrocyte transplantation – ACT for short?
Arthroscopic ACT is a promising method for treating localised cartilage defects. During the first surgical procedure, the patient’s own cartilage cells (chondrocytes) can be removed.
In a complex procedure, the cartilage cells are then cultured for a defined period of time to produce three-dimensional spheroids containing around 200,000 cartilage cells with a diameter of 0.5-0.7 mm. These are then implanted into the cartilage defect in a second surgical procedure. You can find more information on this page.
Another special feature of this procedure is that the cartilage cells are grown and the spheroids are produced using only the patient’s own blood serum. This avoids any foreign reactions or side effects.
The cost of this procedure should be discussed with your health insurance company in advance.
What happens after cartilage damage is treated?
The cartilage regenerates during the exercise treatment. Passive movement with a motor splint should be performed at least four to six hours a day for four weeks.
If movement is useful, which sports are recommended?
Complete rest of the operated leg does not make sense and is also impossible in the case of the hip joint, since the joint is already fully loaded when sitting. To „massage“ the cartilage, the patient should regularly use an ergometer (bicycle with no great resistance). For about nine to twelve months, the patient shouldn’t participate in sports involving stress, such as jogging and impact sports.
Glucosamine and chondroitin sulfate may be taken orally or injected directly into the hip joint for the first twelve months after surgery.
Further therapy options
Minimal-invasive treatment
In recent years, there has been an increased focus on muscle-sparing and joint-preserving orthopedic techniques. The main reason is the young age of the patients and their higher activity level. After surgery, they want to return to their normal daily activities as soon as possible. Minimally invasive surgery (MIS) offers the opportunity to improve the patient’s quality of life through rapid postoperative mobilization and active recovery.
How is minimally invasive hip surgery performed?
In hip surgery, a customized skin incision is chosen that allows access to the hip joint without damaging the muscles.
Hip arthroscopy requires only 2-4 small skin incisions to allow treatment of many joint pathologies with adapted instruments. This allows for the treatment of impingement, labral tears, synovitis, removal of free joint bodies, and cartilage therapy.
What do extensive pathologies require?
Extensive pathologies sometimes require a short skin incision for adequate treatment. This can be done with arthroscopic assistance to minimize soft tissue trauma during surgery. It is also possible to cover localized cartilage damage with a small cap (HemiCap), avoiding the need for total joint replacement. These minimally invasive treatments allow early mobilization of the patient and a quick return to normal daily activities.
Arthroscopic treatment
What is arthroscopy and why are few orthopedic surgeons performing it?
Arthroscopy of the hip joint has become increasingly popular in recent years for the treatment of hip disorders. This procedure has evolved significantly over the past decade in terms of access and surgical techniques, and special instruments can now be used to treat conditions in and around the joint. However, this procedure is only performed by a few orthopedic surgeons in Germany because of the extensive and complex nature of this type of surgery.
What are the benefits of hip arthroscopy?
The advantage of this minimally invasive technique is that it spares the muscular structures around the hip joint that can be damaged by open surgery. In addition, there is less pain in the hip and groin after surgery, allowing for a quicker recovery.
What are the typical indications for arthroscopy?
Typical indications for arthroscopy of the hip joint are diseases of the labrum, femoroacetabular impingement (FAI), cartilage damage of the hip joint with cartilage treatment (chondrocyte transplantation, AMIC procedure, microfracture, etc.) and the structures surrounding the hip joint (tendons, bursa). The symptoms are sometimes expressed as pain in the groin when sitting in a car, during work or during sports activities.
What are the preliminary clinical tests?
The exact examination includes special imaging (x-rays, magnetic resonance imaging (MRI) with contrast) to determine the cause of the symptoms. This allows the surgical procedure to be planned and performed with precision.
What are the benefits of arthroscopy during surgery?
Arthroscopy of the hip allows visualization of both the inside (central compartment) and outside (peripheral compartment) of the joint during surgery. Diseases can be treated at the same time. Structures around the hip joint can also be repaired (bursitis, tendon pathologies). During the operation, the hip joint is carefully widened under anesthesia so that the X-ray can be inserted into the joint. With the help of the camera and various instruments, the diseases can then be optimally treated.
An individualized aftercare plan is developed for each patient, depending on the surgery performed. This plan is given to the patient and the physiotherapist who will continue the treatment. This ensures standardized and patient-specific follow-up care, regardless of where the patient lives.
Endoprosthetics
When is hip replacement considered?
Osteoarthritis of the hip joint with damage to the articular cartilage often causes pain at rest or during physical activity. This limits quality of life. When cartilage-preserving treatments (injections, arthroscopy, etc.) are no longer possible, an endoprosthetic replacement of the hip joint should be considered.Arthritis of the hip joint with damage to the joint cartilage often leads to pain at rest or during physical activity. This limits quality of life. When cartilage preserving treatments (injections, arthroscopy, etc.) are no longer possible, endoprosthetic replacement of the hip joint should be considered.
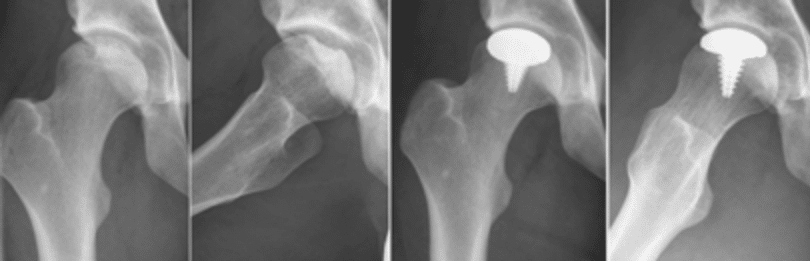
Fig.1: Typical arthrosis with loss of cartilage and joint space (left) Postoperative images after hip replacement (center, right)
What are the surgical options?
Currently, there are several surgical procedures available to replace both components of the joint and reduce pain while improving the patient’s quality of life. Hip arthroplasty is a well-established procedure for the treatment of advanced hip osteoarthritis. Uncemented and cemented hip endoprostheses have been implanted for years with very good results, with the expectation of a 15-20 year lifespan before replacement surgery may be required.
What additional methods have been introduced in recent years?
Alternative treatment concepts have been developed in recent years, allowing many hip arthrosis cases to be treated with bone-sparing implants. In many cases, implants can be inserted using a minimally invasive anterior/anterior or antero-lateral technique, allowing for much faster postoperative mobilization.
What are short stem prostheses?
Bone-sparing implants are short stem prostheses that require less bone resection than standard endoprostheses. These bone-sparing implants often allow for the placement of a conventional implant in future replacement surgeries, so these types of endoprostheses can be considered „prosthesis before prosthesis“.
Figure 2: Modern surgical treatment options for hip arthrosis (left) and two short shaft prostheses (center, right).
Why has the implantation of a surface replacement prosthesis been discouraged in recent years?
In recent years, the implantation of surface replacement prostheses has not been recommended. In many cases, they lead to severe abrasion of the metal-on-metal bearing couple, resulting in metallosis, pseudotumors, hypersensitivity and neurological problems. Therefore, affected patients should urgently undergo serum metal ion monitoring and other tests to detect serious complications at an early stage. We perform such screening examinations in our center.
What happens after the surgery?
Immediately after surgery, patients are mobilized with full weight-bearing on the affected joint and can continue their treatment after a few days. With the Fast Recovery or Fast Track procedure, a quick return to normal activity is possible. Hospital stay can also be reduced to a few days.
When is a partial prosthesis recommended?
In special cases with localized cartilage defects of the femoral head, a partial prosthesis with a HemiCAP can be performed to cover only the affected area – followed by a return to full activity.
What are the prerequisites and what surgical techniques are used?
The prerequisite for such a procedure is an accurate diagnosis using x-ray and MRI to assess the extent of cartilage damage. These can also be implanted using minimally invasive techniques, allowing patients to be discharged from the hospital after a few days.
Patients are mobilized with full weight bearing on the affected joint immediately after surgery. After a few days, they are discharged for further treatment.
MAKO robotics
What is MAKO Robotics?
„Accuracy to the millimeter“ is especially important in joint surgery, where delicate parts such as the hip or knee joint need to be operated on. Surgery on such complex joint structures, where bones lie close to tendons, ligaments and nerves, requires absolute precision. That is why we rely on the most advanced technology in hip surgery. One of the most advanced is called Mako SmartRoboticsTM®. Read more about its methodology and benefits on this page.
Replacing a prothesis (revision)
When does a prosthesis need to be replaced?
As a result of the large number of hip prostheses implanted in recent decades, the number of hip replacement surgeries is increasing due to the incidence of prosthesis loosening. This may be due to the long service life of the prosthesis or other causes. In many cases, no cause of loosening can be found after about 20 years of use, which is called aseptic loosening. A possible reason for early loosening of the prosthesis is the abrasion particles of the polyethylene plastic of many acetabular cups, which can degrade the bone in the area of the stem or the cups. Rarely, septic loosening due to bacterial infection may occur as an early infection after implantation. However, if this occurs years later, it is a low-grade infection.
What exactly can become loose?
In general, the hip stem, acetabulum, or both can loosen, requiring replacement surgery. Depending on the size of the bone defect, either conventional endoprostheses or special implants are required for a successful replacement.
For the acetabulum, these are traditional acetabular components that are either pressed into the pelvic bone (press-fit cups), screwed into the pelvic bone (screw cups), or cemented into place. For larger defects, the fracture is usually filled with bone graft or foreign bone and a revision cup with screw fixation is selected.
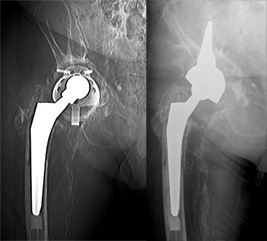
Figure 1: Aseptic acetabular loosening treated with cup reconstruction with foreign bone and revision cup implantation.
Fig. 2: Complex revision of multiple previous acetabular fractures with tilted and loosened revision cup. Switch to modular partial pelvic replacement (Lumic, Implantcast).
In the stem area, standard grade stems are used primarily for smaller defects, and revision systems with longer stems and the option of screw anchorage are selected only for larger defects involving the proximal part of the femur.
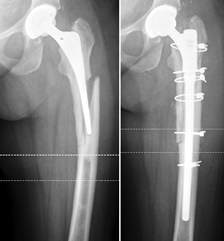
Fig. 3: Early aseptic loosening of a short stem prosthesis after 4.5 years, which was replaced with a standard grade prosthesis.
What happens in the case of a bacterial infection?
In cases of septic loosening caused by bacterial infection, a two-stage exchange is required, in which bone cement with antibiotic (as a placeholder) is inserted until the defect has healed. After 6-8 weeks, the hip arthroplasty can be successfully replaced under antibiotic therapy.
What is the diagnosis here?
In many cases, a 3-phase skeletal scintigraphy is performed in addition to conventional radiologic studies (conventional x-rays). If a septic loosening is suspected, an inflammation scintigraphy (leukocyte scintigraphy) in combination with a puncture of the joint should be discussed for further diagnosis. SPECT-CT is also available for a highly specialized analysis of prosthesis pain.
What does mobilization look like?
In many cases, early functional mobilization under full weight-bearing is performed, depending on the size of the defect and the components replaced. For larger defects or slightly reduced bone quality, partial weight bearing should be used for 6 weeks.